Best orthodontic Adhesive Cement USA IOS

IOS: The One-Stop Shop for the Best Orthodontic Adhesives

| Table of Contents | |
|---|---|
When it comes to orthodontics, choosing the right adhesive is crucial. Orthodontic adhesives are essential for bonding brackets and tubes to teeth during treatment. With so many options available in the market, it can be hard to know which adhesive is right for you. That's where IOS comes in - we offer the best orthodontic adhesives that are specially designed to meet your needs.
In this article, we will cover everything you need to know about orthodontic adhesives. From what they are and why quality matters in choosing them, to the various types of adhesives and their application techniques. We will also provide tips on how to use and store them properly, and the safety concerns associated with using orthodontic adhesives.
So if you're looking for a one-stop-shop for all your orthodontic adhesive needs, look no further than IOS!
Introduction
Bonding failure of orthodontic brackets and tubes is an unpleasant situation for both orthodontists and patients, causing increased appointments and prolonged chair time (REF)
Although the market has different adhesive systems, IOS envision was to design and manufacture the best and highest quality orthodontic adhesives. IOS offers a wide range of adhesives and cements for all your orthodontic needs.
What are orthodontic adhesives
When undergoing orthodontic treatment, braces are attached to the teeth using specialized materials called orthodontic adhesives. These adhesives are used to bond the bracket base to the tooth surface, providing precise control of tooth movement. Orthodontic adhesives come in different types, such as resin-based adhesives and glass ionomer cements, depending on factors such as bracket type, tooth restoration, attachments, and individual patient needs. Proper selection of high-quality orthodontic adhesives is crucial for successful treatment outcomes.
Importance of using quality orthodontic adhesives
The secret to manufacturing an ideal (NOT STRONGEST) orthodontic adhesive lies in balancing the bonding strength during treatment with the debonding strength at the end of the treatment.
- During treatment, the adhesive should have an optimal bond strength to withstand both chewing and orthodontic forces. Research has shown that the minimum shear bond strength should range between 6 and 8 MPa to avoid bracket deboning during application of orthodontic forces. (REF)
- During debonding, the adhesive should allow the easy removal of the bracket. This avoids the possibility of damaging the dental enamel or the dental restoration.
Thus, Investing in quality orthodontic adhesives can save time, money, and improve patient satisfaction.

Why choose IOS for orthodontic adhesives
At IOS, we have years of experience in manufacturing a wide range of orthodontic adhesives that have been rigorously tested for strength and durability. Tests are done both In-vivo and In-vitro under different loads and conditions, different brackets, different appliances and different techniques "Direct bonding vs. Indirect bonding".
Our R&D team always utilizes advanced technology to achieve optimal bond strength and long-lasting results.
Types of Orthodontic Adhesives
There are various types of adhesives available at IOS, including light-cured composite resin, self-cured composite resin and glass ionomer cements. Light-cured adhesives are the most commonly used and require a special dental light to set. Self-curing adhesives are activated by mixing two compounds. Glass ionomer cements are ideal for cementing single bands and appliances.
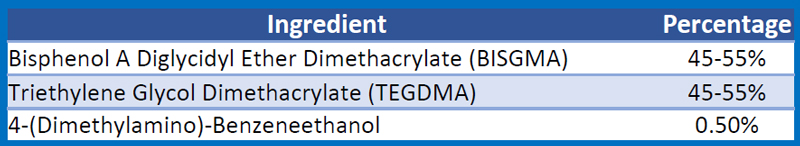
1. Chemical cured composite resin
This system has two parts; a resin paste to be placed on the bracket base and a liquid primer to be placed on the teeth. The resin will start to set once in contact with the primer. The clinician has a period of 20 seconds to properly position the bracket and the bracket will be ready for complete wire load in 4 minutes.
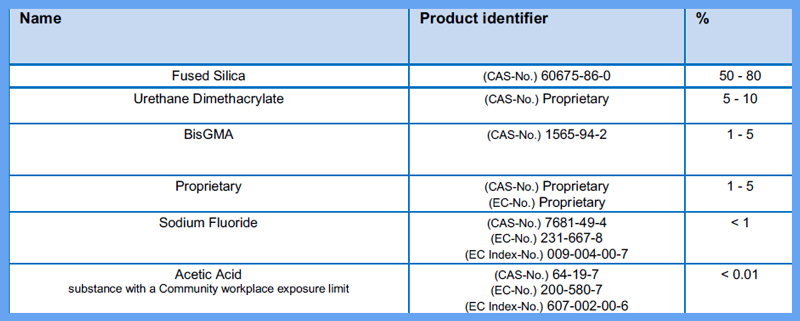
2. Light cured adhesive
Unlike the chemical composite, the light cured composite has a photoinitiator to start the polymerization process. This will give the clinician extra time to place more than one bracket at the same time with the option to reposition the bracket if not in the desired position.
The photoinitiator requires the right wavelength and intensity of curing light to work. The International Organization for Standardization has recommended a minimum intensity of 300 mW/cm2 with a wavelength bandwidth of 400-515 nm on the tip of the blue light curing device (REF).
Light cured composite resins have good strength and durability for direct, and indirect bonding, metal brackets and porcelain brackets as well.
3. Glass ionomer cements
Glass ionomer cements are a popular choice for orthodontic bonding due to their excellent adhesion to both enamel and dentin. The cement releases fluoride, which helps protect against decay and can strengthen the tooth structure. Additionally, they have a low viscosity, allowing for easy application and adaptation to the tooth surface. Biocompatible and safe for use in the mouth, glass ionomer cements are commonly used for bonding orthodontic brackets and bands.
Factors to consider when selecting the Best Orthodontic Bracket Adhesive
When selecting the best orthodontic bracket adhesive, there are several factors to consider.
- Bond strength is critical to ensure effective bonding of the brackets, tubes and appliances,
- Viscosity affects how easily the adhesive can be placed.
- Curing time is another important consideration as it affects bonds strength (REF).
- Color, it's essential to choose an adhesive that matches the color of teeth, and
- Biocompatible for safe use in the mouth.
Bond strength
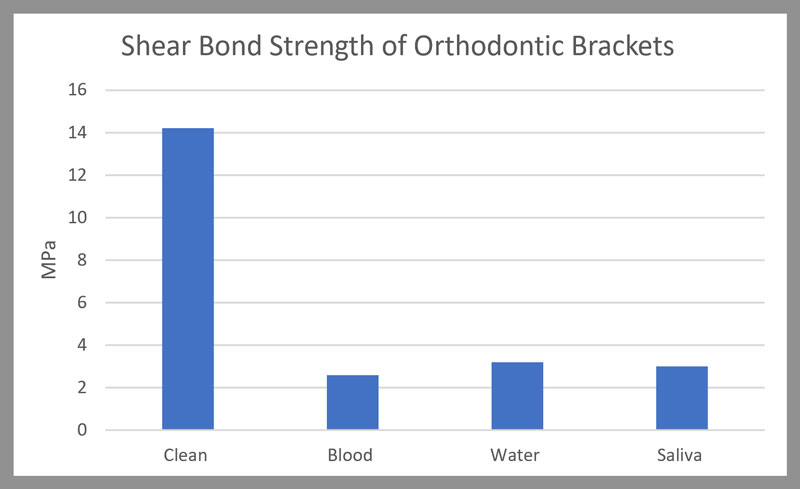
The bond strength of orthodontic adhesive is a crucial factor that determines their effectiveness during treatment. Research has shown that a minimum bond strength of 5.9–7.9 MPa could result in successful clinical bonding (REF). IOS TRUEBOND LC has a shear bond strength of 14.00 MPa compared to 12.18 MPa of Transbond XT. It is important to understand that preferable bond strength for restorative dentistry is different from that in orthodontics. In restorative dentistry, the higher bond strength is more desirable, whereas in orthodontics, optimum bond strength is preferred. This is important to ensure easy bracket removal at the conclusion of the treatment without causing damage to the enamel.
Setting time
When it comes to orthodontic adhesive, the setting time is an essential factor to consider. Different types and brands of adhesives have varying setting times. Shorter setting times may be more convenient for busy practices, while longer setting times allow for more precise placement and adjustment of brackets. Self-curing adhesives use chemical reactions to set, while light-cured adhesives use UV light. It's important to choose an adhesive with the appropriate setting time based on the specific needs of your patients and practice. IOS TrueBond LC implements photoinitiators with high light sensitivity. This will not only reduce the curing time, but also allow the cure under impermeable metal materials.
Fluoride release
Using orthodontic adhesive with fluoride release can offer several benefits for patients undergoing treatment. These adhesives may help prevent tooth decay, strengthen enamel, and reduce the risk of white spot lesions. All TrueBond adhesives are fluoridated adhesive that release fluoride without affecting the bond strength (REF)
Handling characteristics
The handling characteristics of orthodontic adhesives play a crucial role in their successful application. Different types of adhesives have varying handling characteristics, from low viscosity "thinner" to highly viscous "thicker". IOS manufactures TrueBond in medium viscosity to accommodate the everyday need of the orthodontist. Also, studies have shown that the viscosity of orthodontic primer was associated with the type and amount of monomer. The viscosity of orthodontic adhesive primer was also found to be influenced by different temperatures. Increases in the temperature resulted in reduced viscosity for each of the orthodontic adhesive primers. A low-viscosity primer will allow better flow into the enamel surface to create deeper resin tags
TIP: in cold weather, warming the composite will decrease the viscosity and make it easier to apply.
Preparation for Bonding with Orthodontic Bracket Adhesive
Teeth should be clean and dry before bonding with orthodontic adhesives to get optimum bond strength. Proper isolation techniques ensure the tooth surface stays dry. You can use a simple cheek retractor (IOS 19-121-103) or get a sophisticated Nola dry field system ( IOS 19-141-101)
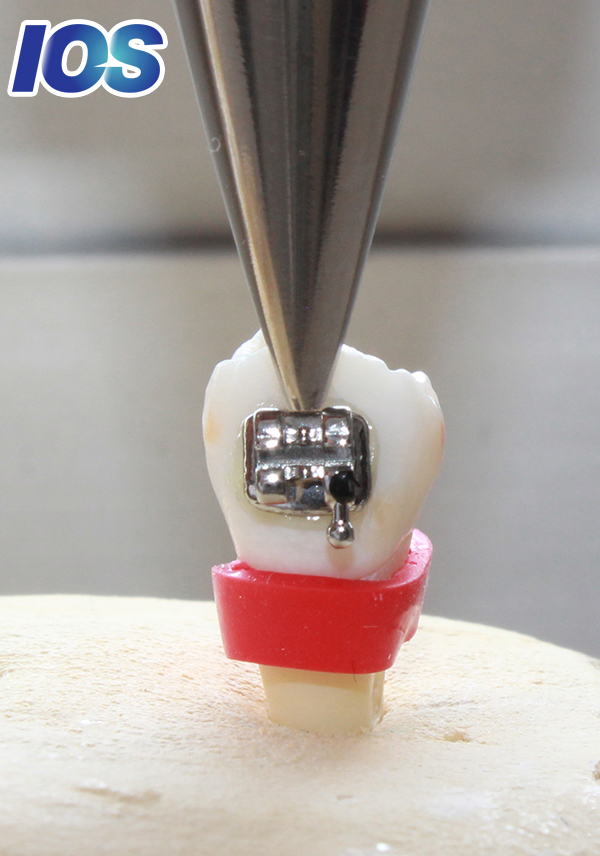
Surface preparation and bracket bonding
Proper surface preparation is critical for successful orthodontic bonding. The teeth must be free of plaque and debris before etching the enamel. After etching, the tooth should be clean from water, blood, saliva and other contaminants. Research has shown that Water and saliva contamination of enamel during the bonding procedure lowers bond strength values up to 80%. (REF).
Cleaning
Proper cleaning is crucial before bonding orthodontic adhesives to ensure the adhesive bonds securely. The tooth's surface must be thoroughly cleaned to remove any debris or plaque that may interfere with the bond. Cleaning could be achieved with:
- A dental handpiece with a low-speed attachment and a fine diamond,
- A prophy cup with pumice or
- An air polisher with fine grade powder.
After cleaning, rinse the tooth surface with water and dry it completely before applying the bond for best results.
Preparing the working area
Proper preparation of the working area is crucial for successful bonding with orthodontic adhesives. To begin, the area should be free of any debris or moisture that may interfere with the bonding process. Using a dental dam or cotton rolls to isolate the teeth and gums can prevent contamination. Cleaning and etching the tooth surface using an appropriate solution will improve adhesive retention, and ultimately ensure a strong bond between the bracket and the tooth.
Antisialagogue agents
Adequate moisture control is crucial during orthodontic bonding to keep etched teeth dry and free from saliva contamination. Antisialagogue agents can be used to reduce saliva flow. This helps to keep teeth dry and improve the adhesion of the orthodontic appliance. The most common medication used to control salivation is Atropine as tablets 0.4-1.6 milligrams.
However, there is no conclusive scientific evidence to support the use of antisialogogues during dental procedures or to reduce bond failure and chair time (REF)
Enamel pretreatment
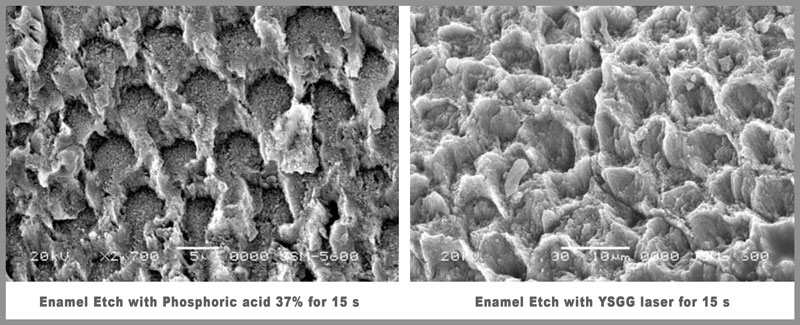
Proper enamel pretreatment is a critical step in ensuring successful bonding with orthodontic adhesives. The traditional way is to use phosphoric Acid 38% for 15 seconds. This process will create a rough surface that is enough for optimal bonding strength.
However, there are alternative methods available that can be less invasive and more comfortable for patients. Air abrasion and laser etching are two such alternatives that have gained popularity in recent years. These methods use a stream of fine particles or a laser to prepare the tooth surface, respectively and can reduce the risk of enamel damage or sensitivity. Consult with your orthodontist to determine the best method for your individual needs.
Laser etching
Recently, lasers have been considered as potential replacements for conventional etching. Laser etching is a modern method of surface preparation that is painless and does not involve vibration or heat, making it highly attractive for routine use. The process takes 15 seconds for each tooth and will create small indentations on the tooth surface, which increases the surface area for bonding and allows for better adhesion of the adhesive. The two most common lasers in use today are Er:YAG:2940 nm and Er: Cr: YSGG; 2,790 nm
Sandblasting
Sandblasting is a widely-used technique for preparing teeth for bonding with orthodontic adhesives. It involves using a high-pressure stream of abrasive particles to remove debris and contaminants from the tooth surface, creating a rougher surface that allows for better adhesion. When done correctly with the use of a low viscosity primer, sandblasting can improve the effectiveness of orthodontic adhesives (REF)
Application Techniques for Orthodontic Adhesives
The orthodontic bracket adhesive could be applied in two different techniques:
1.Direct bonding technique
The direct bonding technique is the most common method used for applying orthodontic adhesives. It involves placing a small amount of adhesive on each tooth and then attaching the brackets to them. This technique will take longer time, but the advantages are:
- The bracket bases were fitted closer to the tooth surface (which improved bond strength),
- Easier to work clean and to remove excess adhesive flash around the bracket bases, and
- The bonding adhesive constantly filled out the entire contact surface of the brackets
2.Indirect bonding technique
Indirect bonding technique has become an increasingly popular option since its introduction by Silverman and Cohen in 1972 (REF). This technique will reduce clinical time, improve accuracy and efficiency in placing brackets, and will enhance patient comfort. It involves creating a custom tray for each arch and applying the adhesive to the tray instead of directly to the teeth. it is highly recommended to lingual braces. However, it is essential to use the right adhesive material and follow proper preparation and application techniques to ensure successful treatment outcomes.

Maintenance of adhesives in orthodontics
In general, light-cured orthodontic adhesive is more stable than chemically-cured orthodontic adhesive that is more sensitive to storage conditions and thus has lower shelf life. This is because of the unstable benzoyl peroxide initiator that is a component of their curing system. Consequently, the storage of the adhesive in the dark and under refrigeration prolongs significantly its shelf life by slowing the decomposition of the initiator.
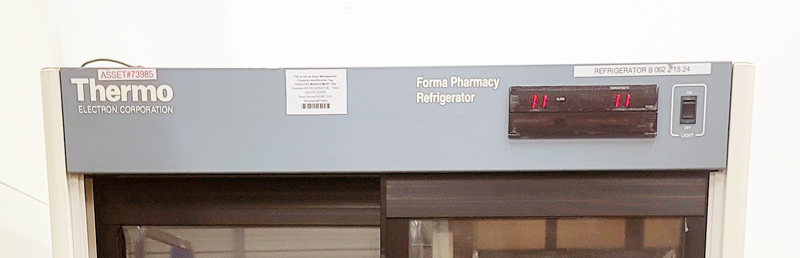
Also, When stored in the refrigerator, the adhesive should be allowed to return to room temperature before use. This will ensure that the material does not experience water condensation, which will both weaken the adhesion, and that, it has the proper viscosity and setting rate.
Ensuring proper storage of the orthodontic adhesives is crucial for successful treatment outcomes. Regular check the expiration date and use older syringes before opening new ones.
Always place back the TrueBond tube cover after each use.
Removal of Orthodontic Adhesives
Removing orthodontic adhesives requires a delicate touch to avoid damaging the tooth or surrounding tissue. After removing the bracket, the orthodontist can either use an adhesive removing plier to clean the tooth ( IOS 18-440) or use a carbide finishing bur ( IOS 19-732-203). After debonding, the teeth may require polishing and smoothing to remove any residual adhesive. It's best to leave this job to a professional orthodontist for optimal results.
Conclusion
When it comes to orthodontic adhesives, ideal is key. Poor-quality adhesives can lead to bracket failure, prolonged treatment time, and other complications. At IOS, we understand the importance of using high-quality adhesives in orthodontic treatment, which is why we offer a wide range of options to suit your needs. Whether you prefer composite resins or glass ionomer cements, we have you covered. Plus, our experienced team is always available to help you select the right adhesive for your needs and provide tips for proper use and maintenance. To learn more about our orthodontic adhesive options and why IOS is the best choice for your needs, visit our website or contact us today.
Frequently Asked Questions
What are some of the key features to look for in orthodontic adhesives?
When selecting orthodontic adhesives, it is important to look for high bond strength to ensure that braces stay in place. Adhesives that release fluoride can also help prevent tooth decay during treatment.
Additionally, adhesives that are easy to handle and cure quickly can make the application process smoother. It is also important to consider any allergies or sensitivities the patient may have when selecting an adhesive. Overall, a good orthodontic adhesive should provide strong bonds, promote oral health, and be easy to use.
References
Demirovic K, Slaj M, Spalj S, Slaj M, Kobaslija S. Comparison of Shear Bond Strength of Orthodontic Brackets Using Direct and Indirect Bonding Methods in Vitro and in Vivo. Acta Inform Med. 2018 Jun;26(2):125-129. doi: 10.5455/aim.2018.26.125-129. PMID: 30061785; PMCID: PMC6029916.
Omidi BR, Gosili A, Jaber-Ansari M, Mahdkhah A. Intensity output and effectiveness of light curing units in dental offices. J Clin Exp Dent. 2018 Jun 1;10(6):e555-e560. doi: 10.4317/jced.54756. PMID: 29946413; PMCID: PMC6012498.
Almeida LF, Martins LP, Martins RP. Effects of reducing light-curing time of a high-power LED device on shear bond strength of brackets. J Orofac Orthop. 2018 Sep;79(5):352-358. English. doi: 10.1007/s00056-018-0146-0. Epub 2018 Jul 31. PMID: 30066016.
Raji SH, Banimostafaee H, Hajizadeh F. Effects of fluoride release from orthodontic bonding materials on nanomechanical properties of the enamel around orthodontic brackets. Dent Res J (Isfahan). 2014 Jan;11(1):67-73. PMID: 24688563; PMCID: PMC3955318.
Sfondrini MF, Fraticelli D, Gandini P, Scribante A. Shear bond strength of orthodontic brackets and disinclusion buttons: effect of water and saliva contamination. Biomed Res Int. 2013;2013:180137. doi: 10.1155/2013/180137. Epub 2013 May 15. PMID: 23762825; PMCID: PMC3671238.
Sfondrini MF, Gatti S, Scribante A. Effect of blood contamination on shear bond strength of orthodontic brackets and disinclusion buttons. Br J Oral Maxillofac Surg. 2011 Jul;49(5):404-8. doi: 10.1016/j.bjoms.2010.06.011. Epub 2010 Jul 23. PMID: 20655131.
Kuijpers MA, Vissink A, Ren Y, Kuijpers-Jagtman AM. The effect of antisialogogues in dentistry: a systematic review with a focus on bond failure in orthodontics. J Am Dent Assoc. 2010 Aug;141(8):954-65. doi: 10.14219/jada.archive.2010.0309. PMID: 20675421.